Table of Contents
Full arch implant-supported restoration techniques have undergone continuous development in recent years and have gradually become a widely adopted clinical solution for edentulous rehabilitation.
This case report demonstrates the application of a fully digital workflow for full-arch implant-supported rehabilitation in an edentulous maxilla utilizing five implants. In the past, it is usually a big challenge to capture the implant position accurately in an easy way, but with the Aoralscan Elite, which adopt the intraoral photogrammetry, it not only improves the accuracy, but also smooth the clinical treatment process, enhances the efficiency and patient comfort.
In this case, pre-op CBCT analysis confirmed adequate alveolar bone volume and quality for implant placement. A guided surgical approach was employed to achieve optimal implant positioning. Post-op data acquisition—including intraoral scans, facial scans, and dynamic mandibular tracking with a screw-retained bite fork—enabled precise determination of the occlusal plane and a reproducible centric relation based on functional mandibular movements. An immediate-loading provisional prosthesis was virtually designed and fabricated using the high-precision AccuFab-F1 3D printer, capable of printing high-filled ceramic resin with a resolution of 25 microns. Following isopropyl alcohol cleaning, support removal, the printed model was used for clinical try-in and immediate provisional restoration. This case highlights the accuracy, efficiency, and clinical feasibility of a fully digital protocol for All-on-five immediate-loading implant rehabilitation.
1. Pre-op evaluation: data collection and case analysis
Before treatment, the patient was using a removable denture, with one remaining tooth in the maxilla and three remaining teeth in the mandible [Fig. 1-4]. Intraoral examination revealed a favorable oral condition for implant surgery, with adequate alveolar bone volume, healthy soft tissues, and no evident signs of inflammation or pathology. The overall oral environment was stable and well-suited for implant placement.
The patient reported dissatisfaction with the removable prosthesis due to its poor retention during mastication, which compromised chewing efficiency and comfort. Additionally, the need for daily removal and cleaning was perceived as inconvenient.
After comprehensive evaluation, the doctor proposed a fixed implant-supported prosthetic plan involving the placement of six implants to achieve long-term functional and esthetic rehabilitation. However, due to financial considerations, the patient opted to proceed with implant-supported fixed restoration in the maxilla only at this stage. Restoration of the mandible may be considered in the future depending on the patient’s circumstances.
Fig (1-4): Pre-op images
The patient underwent CBCT examination [Fig.5]. The imaging revealed partial edentulous in the bilateral posterior maxillary regions, accompanied by varying degrees of alveolar ridge resorption. The maxillary bone density is within an acceptable range, with intact cortical bone continuity and no significant destruction of the cancellous bone structure.

Fig 5:Pre-op CBCT images
2. Treatment Plan: All-on-five implant
The primary challenge in this case was the lack of a pre-op occlusal record. Combined with the loss of vertical dimension, this made it impossible to accurately establish the correct jaw relationship.
Based on the patient’s intraoral condition and personalized prosthetic needs, doctor conducted a comprehensive assessment of intraoral scan data, facial scan data, and CBCT imaging. By utilizing a facial scanner in combination with reference point alignment, the optimal jaw relationship was established, providing a reliable foundation for the digital design and precise fabrication of the final prosthesis. A full-arch implant-supported restoration plan was finalized, involving the placement of six implants in the alveolar bone to complete a fully digital restorative workflow.
Due to insufficient primary stability of the implants, the fabrication of the All-on-six prosthesis was postponed until osseointegration was achieved following a submerged healing period[Fig.6].Therefore, a restoration was temporarily fabricated on five implants, while the sixth implant will be restored after achieving sufficient osseointegration.

Fig:6 Post-op CBCT images
3. Treatment Process
3.1 Intraoral scanning to capturing the implant position
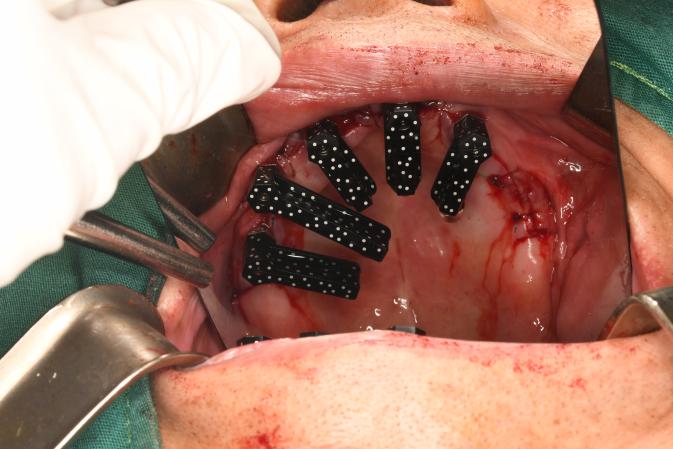
Following implant surgery [Fig.7-8], the clinician used the Aoralscan Elite to capture digital impressions. The process began with an edentulous scan. In cases where excessive bleeding was present, the soft tissue could appear overly reflective or shift during scanning, potentially compromising data accuracy. To address this, a cap scanbody may be employed, ensuring efficient data acquisition with high accuracy.
Fig. 7, 8: Post-surgical intraoral scan data
Next, coded scanbodies were installed, the scanned data can then be converted and transfer to third-party libraries. [Fig. 9,10]
Figs. 9,10: Intraoral scans acquired with Aoralscan Elite using coded scanbodies
3.2 Optimal jaw relationship determination using MetiSmile-MR
As a revolutionary advancement, the MetiSmile-MR is the first facial scanner to unify facial data acquisition with dynamic jaw tracking, setting a new standard in digital dentistry.
In the digital reconstruction process for edentulous patients, establishing an accurate and stable jaw relationship is fundamental to achieving both functional and esthetic rehabilitation. The patient is guided to perform approximately 30 times opening and closing movements, enabling the system to capture mandibular motion and record the most repeatable functional trajectory [Fig.11].

Fig11: 30 cycles of mandibular movement. The green position represents the patient’s rest position. During these 30 cycles, it helps prevent a protrusive movement and facilitates accurate capture of the mandibular trajectory.
The software then identifies key landmarks, sets up a coordinate system based on these reference points. Doctors can adjust the vertical distance to find the optimal occlusal height. For the horizontal relation, the software calculates the intersection of the motion path with the horizontal plane, giving the centric relation and myofascial points for the doctor’s reference. Users can also easily check the occlusion with the four cross-sectional planes along the dental arch, and the software will show the interocclusal measurements [Fig 12].

Fig. 12: Analysis of the optimal jaw relationship
3.3 Design and 3D printing
After designing, using the AccuFab-F1 to print the restoration. The AccuFab-F1 is the latest 3D printer developed by Shining 3D, it is featuring a dual-heating system, enables the stable and efficient processing of high ceramic-filled resins material. The system achieves a printing resolution as fine as 25 μm, ensuring high dimensional accuracy and surface quality. For full-arch All-on-X prosthetic workflows, the printer is capable of completing within approximately 10 minutes [Fig. 13].

Fig. 13: All-on-five implant-supported prosthesis
3.4 Try-in
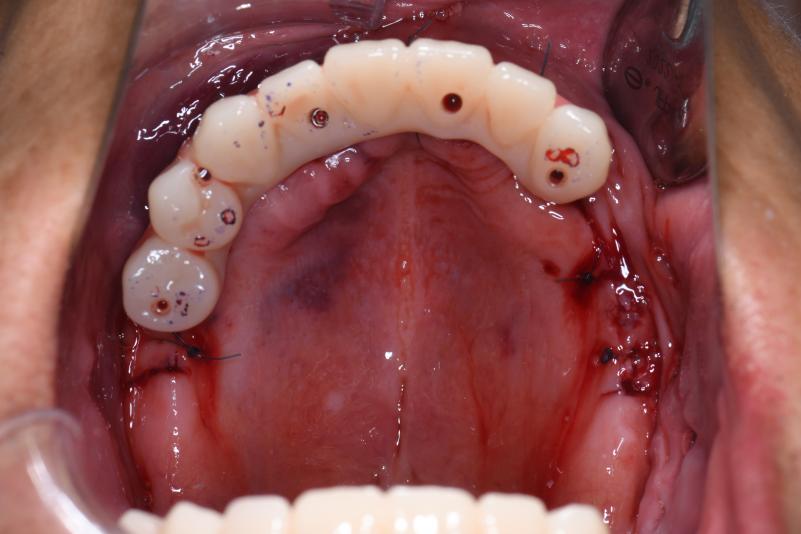
This case successfully achieved full-arch rehabilitation using five implants. The try-in phase was highly satisfactory for the patient [Figs. 14, 15]. The entire process proceeded smoothly, requiring minimal occlusal adjustments. The temporary restoration was delivered within one day, making the treatment process efficient and well experienced.
Fig 14, 15: The try-in process intraorally.
4. Discussion
Conventional full-arch implant impressions and occlusal registrations in edentulous patients present several challenges. Achieving accurate soft tissue capture can be difficult due to tissue mobility. Blood and moisture often interfere with impression materials, compromising detail. Establishing a stable and reproducible jaw relationship is complicated by the absence of natural teeth, leading to potential errors in occlusal vertical dimension and centric relation.
By utilizing the Aoralscan Elite’s photogrammetry technology (IPG) alongside its facial scanner jaw motion function, an optimal maxillomandibular relationship was captured. This enabled a fully digital implant workflow with high-precision positioning and scanning, assisting clinicians in achieving more accurate and predictable treatment outcomes.
 ENG
ENG